At a Glance
- The CDC no longer recommends routine meningitis A,C,Y,W vaccination for all adolescents
- Cases of invasive meningococcal disease jumped to 500+ in 2024, the highest since 2013
- Doctors warn the change could reverse the 90% drop in cases seen after the 2005 universal recommendation
- Why it matters: Teens and college students in dorms remain at high risk for the fast-killing brain infection
The Centers for Disease Control and Prevention has quietly removed the meningococcal A,C,Y,W vaccine from its list of universally recommended adolescent shots, a move that physicians fear will open the door to rising cases of the rapid, often fatal bacterial infection that once devastated teen populations.
Meningitis Cases Surge After Years of Decline
Since the CDC first urged routine vaccination of 11- to 12-year-olds in 2005, annual U.S. meningococcal disease cases fell by 90%. That two-decade downward trend has reversed: reported infections climbed sharply after 2021 and reached more than 500 in 2024, the highest total since 2013.
Doctors attribute the upswing to:
- Mutations in circulating bacteria that increase virulence
- Slipping adolescent vaccination coverage, especially for the 16-year-old booster
- Waning population immunity as vaccine protection fades over time
New Guidance Limits Vaccine Access
Under the revised childhood schedule released by Health Secretary Robert F. Kennedy Jr.’s office, the MenACWY shot is now advised only for “high-risk groups.” Parents who want the vaccine for healthy teens must request it through a process the CDC labels “shared clinical decision making.”
High-risk categories include:
- Teenagers and college-age adults living in communal settings such as dormitories
- People living with HIV
- Individuals with complement deficiencies or asplenia
Dr. Luis Ostrosky, an infectious-disease specialist at UT Health Houston, warned that the policy shift is occurring “just as we are seeing a spike in this Y strain” and could translate into additional deaths.
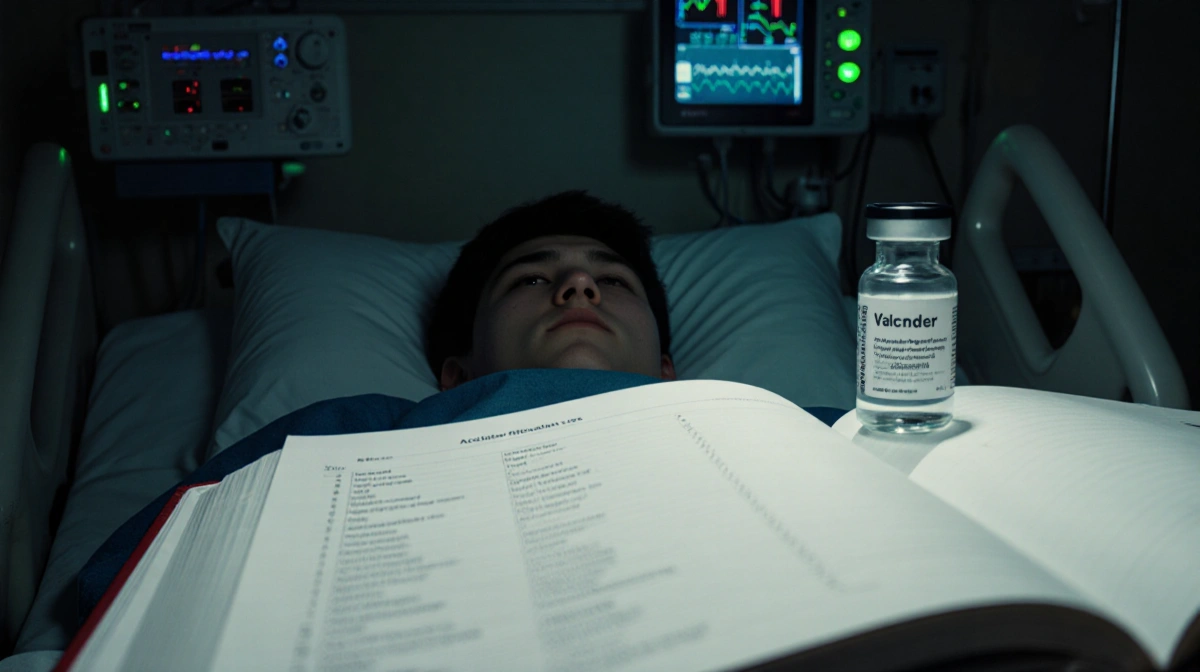
The Disease: Fast, Fierce, Preventable
Neisseria meningitidis bacteria colonize the throat without symptoms in roughly 1 in 10 people, but when they invade the bloodstream or the membranes surrounding the brain the result is meningococcal disease. Progression can be explosive:
- Headache, fever, stiff neck and vomiting appear suddenly
- Brain swelling, limb gangrene and septic shock can follow within hours
- Roughly 15% of patients die even with rapid antibiotic treatment
- Up to 20% of survivors suffer lifelong disabilities-amputations, hearing loss, neurological damage
Dr. Kevin Messacar, a pediatric infectious-disease professor at the University of Colorado Anschutz, called bacterial meningitis “a devastating disease that keeps pediatricians up at night” because early symptoms mimic minor viral illnesses and patients can be “too late to bring back.”
2024 Outbreak Driven by Y Serogroup
Last year’s national alert from the CDC flagged a surge in invasive meningococcal disease caused largely by a Y serogroup strain covered by the previous vaccine recommendations. Demographics of the outbreak:
| Age Group | 30-60 years |
| Race | Disproportionately Black patients |
| Risk Factor | High prevalence among people with HIV |

All FDA-approved MenACWY vaccines include the Y serogroup, underscoring the preventive value doctors believe is being lost.
Experts Criticize “Imported” Policy
Dr. Peter Chin-Hong of UCSF contends that copying Denmark’s selective meningitis vaccination strategy ignores U.S. epidemiology. “You can’t just look at another country’s vaccine approach and photocopy it,” he said, noting that American surveillance data already show rising disease and that the shots have a strong safety record.
Alicia Stillman, co-executive director of the American Society for Meningitis Prevention, serves on a World Health Organization task force aimed at eliminating meningitis globally. She fears the shared-decision model erects barriers for busy families and under-informed clinicians. Her daughter Emily died from meningitis B in 2013, a year before FDA approved that strain-specific vaccine.
Stillman recounted watching providers “not bring it up” and parents miss opportunities because they lacked the knowledge to ask. She predicts the same could now happen with MenACWY.
Safety Data Back Existing Vaccines
More than a dozen randomized trials and decades of real-world evidence support the safety and effectiveness of MenACWY products, according to a 2020 CDC review. The Vaccine Adverse Event Reporting System and the Vaccine Safety Datalink found the most common side effects-injection-site swelling, low-grade fever, headache-were mild to moderate and short-lived.
CDC statements accompanying the new schedule said the agency wants “placebo-controlled randomized trials and long-term observational studies.” Experts counter that withholding a life-saving shot while awaiting placebo trials for a rare, deadly disease is neither ethical nor practical.
Survivors Describe the Aftermath
Katie Thompson contracted an antibiotic-resistant strain during her freshman year of college in 2005, the same month the first MenACWY vaccine won FDA approval. She spent five weeks hospitalized and nearly died. Now 39, Thompson lives outside Charleston, South Carolina, with chronic migraines, vestibular dysfunction and a surgically implanted bladder stimulator.
“It’s pure hell,” she said. “It’s just not a disease that you want to take a risk on. It’s not one that you want to gamble with your child’s life.”
Key Takeaways
- The CDC’s move from universal to risk-based MenACWY recommendation removes automatic adolescent protection
- Physicians warn declining coverage could erase the dramatic incidence drop achieved since 2005
- With 2024 case counts already at an 11-year high, doctors urge parents to request the vaccine through shared-decision appointments
- Meningococcal disease remains rare-about 3,000 U.S. cases yearly-but its speed and severity make prevention critical